
-
 Scotland thrash Tonga in Autumn Nations finale
Scotland thrash Tonga in Autumn Nations finale
-
Three key Irish takeaways from Autumn Nations Series

-
 Imperious Shiffrin swoops to 103rd win at Gurgl
Imperious Shiffrin swoops to 103rd win at Gurgl
-
Schmidt challenges Wallabies to 'roll up their sleeves' after gruesome year

-
 Washington seeking to 'iron out' Trump proposal details with Ukrainians in Geneva
Washington seeking to 'iron out' Trump proposal details with Ukrainians in Geneva
-
South African centurion Muthusamy celebrates 'awesome' Test journey

-
 Brazil 'very concerned' about US naval build-up near Venezuela
Brazil 'very concerned' about US naval build-up near Venezuela
-
Liverpool a 'mess' says Van Dijk

-
 First blind women's T20 cricket World Cup boosts sport
First blind women's T20 cricket World Cup boosts sport
-
France eye Dupont boost for Six Nations defence

-
 McLaren boss apologises to Norris, Piastri for Vegas disqualification
McLaren boss apologises to Norris, Piastri for Vegas disqualification
-
G20 grapples with splintering world order

-
 Verstappen wins big in Vegas with McLarens disqualified
Verstappen wins big in Vegas with McLarens disqualified
-
Muthusamy, Jansen put South Africa on top in second India Test

-
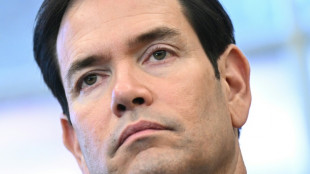
 Rubio lands in Geneva for talks on Ukraine plan
Rubio lands in Geneva for talks on Ukraine plan
-
Norris and Piastri disqualified from Las Vegas GP

-
 Slovenia holds crunch vote on contested assisted dying law
Slovenia holds crunch vote on contested assisted dying law
-
Aonishiki beomes first Ukrainian to win sumo tournament

-
 Holders Australia drawn with New Zealand in Rugby League World Cup
Holders Australia drawn with New Zealand in Rugby League World Cup
-
Vietnam flooding kills at least 90

-
 Muthusamy's maiden Test century powers South Africa to 428-7
Muthusamy's maiden Test century powers South Africa to 428-7
-
Myanmar junta says nearly 1,600 foreigners arrested in scam hub raids

-
 US signals room for negotiation on Ukraine plan ahead of talks
US signals room for negotiation on Ukraine plan ahead of talks
-
Verstappen wins Las Vegas F1 Grand Prix, Norris edges closer to crown

-
 Muthusamy anchors South Africa to 316-6 in second India Test
Muthusamy anchors South Africa to 316-6 in second India Test
-
Vietnam flood death toll rises to 90

-
 US denies pushing Russian 'wish list' as Ukraine plan
US denies pushing Russian 'wish list' as Ukraine plan
-
Harden's 55 leads Clippers win as Pistons streak hits 12

-
 Kim's first top-10 in 14 years as Ballester wins maiden pro title
Kim's first top-10 in 14 years as Ballester wins maiden pro title
-
Gotham crowned NWSL champions after Lavelle breaks Spirit

-
 Trump signals room for negotiation on Ukraine plan ahead of talks
Trump signals room for negotiation on Ukraine plan ahead of talks
-
Head shapes up as solution for Australia's opening woes

-
 Tomorrowland bets on Chinese dance music fans with first indoor event
Tomorrowland bets on Chinese dance music fans with first indoor event
-
England slammed as 'brainless' after first Ashes Test capitulation

-
 Slovenia to hold new vote on contested assisted dying law
Slovenia to hold new vote on contested assisted dying law
-
10 Benefits of Choosing Dental Implants After an Extraction

-
 SKYLINE Announces Q3 2025 Financial Results
SKYLINE Announces Q3 2025 Financial Results
-
'Beer tastes better' for Eramsus after win over Irish

-
 No.1 Jeeno leads by six at LPGA Tour Championship
No.1 Jeeno leads by six at LPGA Tour Championship
-
Neres double fires Napoli top in Italy

-
 Bielle-Biarrey masterclass helps France hold off Australia
Bielle-Biarrey masterclass helps France hold off Australia
-
Pogba returns in Monaco loss as PSG stay top in France

-
 COP30: Key reactions to climate deal
COP30: Key reactions to climate deal
-
What did countries agree to at COP30?

-
 Harden's club-record 55 points leads Clippers over Hornets
Harden's club-record 55 points leads Clippers over Hornets
-
Amazon climate deal a 'win' for global unity but fossil fuels untouched

-
 Boos, blowups and last-minute pause as a chaotic COP30 closes out
Boos, blowups and last-minute pause as a chaotic COP30 closes out
-
Farrell proud of Ireland after 'mad' Test with South Africa

-
 Gaza civil defence says 21 killed in Israeli strikes
Gaza civil defence says 21 killed in Israeli strikes
-
South Africa beat ill-disciplined Irish to end Dublin drought


MDaudit's 2025 Benchmark Report Reveals Ongoing Acceleration of Payer Audits, Troubling Rise in Denials and Outpatient Coding Issues
Annual analysis points to an urgent need to redefine revenue integrity as proactive protection, while strengthening coding integrity and denial prevention measures.
WELLESLEY, MA / ACCESS Newswire / November 18, 2025 / The rate of payer audits accelerated in 2025, with hospital inpatient and outpatient average denial amounts that increased by 14% and 12%, respectively. Denial volumes were also up overall, led by a nearly fivefold increase in Request for Information (RFI) and medical necessity denials for Medicare Advantage plans. The total at-risk amounts, number of claims and average amount per claim increased by 30% in payer audits. Denials related to outpatient coding increased by 26%. These trends send a clear signal to providers that successfully navigating today's complex financial and regulatory landscape requires prioritizing billing compliance, coding integrity, robust denial prevention strategies, and redefining revenue integrity to ensure sustainability.
These were among the key findings of the 2025 MDaudit Annual Benchmark Report released today by MDaudit, an award-winning cloud-based continuous risk monitoring platform for RCM that enables the nation's premier healthcare organizations to minimize billing risks and maximize revenues. The central theme of this year's report is the evolution of revenue integrity from a defensive stance to a proactive discipline that unites charge capture, coding, billing compliance, and denials management within a connected, data-driven framework.
"Reactively fixing denials after they occur or addressing compliance findings after the fact is costly and unsustainable," said Ritesh Ramesh, CEO, MDaudit. "This year's Benchmark Report clearly demonstrates the urgency behind adopting a unified approach to billing compliance, coding integrity, and denial prevention wherein data intelligence and automation are shared across revenue functions, allowing finance leaders to efficiently shift from managing crises to protecting revenue with foresight and confidence."
Key Takeaways
The new Benchmark Report reveals several trends provider organizations should act on now, and identifies where to focus their attention, investments, and process improvements to safeguard income and manage risk as they enter 2026.
1. Rising Denial Rates
The upward trajectory of denial volumes and amounts signals the need for providers to sharpen denial prevention strategies. In 2025, the average denied amount for hospitals rose from $4,730 in 2024 to $5,390 (14%) in outpatient settings, and from $504 to $565 (12%) in inpatient settings. This includes a 70% increase in average denied amounts from RFI and medical necessity denials across all settings. Telehealth-related denials were up 84% in 2025, due primarily to missing information, errors in claim submission, non-covered charges, or duplicate claims
To reverse these trends, provider organizations need to take steps to monitor denial trends by payer, setting, and claim type and reinforce root-cause analysis of denials, such as coding, documentation, and charge capture. Investing in early-warning tools and audit workflows that catch high-risk claims before submission is also recommended.
2. Payer Audits Increase
External payer audits surged again in 2025, with total at-risk amounts and audit cases per customer rising by 30%, and the average amount at risk per claim growing 18%. Of the top payer types, 45% of the at-risk amount was driven by commercial payers, while Medicare and Medicaid accounted for 28%. The average at-risk amount for a payer audit in a hospital setting was approximately $17,000, whereas the average at-risk amount at a professional setting was $1,172.
Intensified payer scrutiny necessitates faster response times, stronger documentation, and proactive risk management. This can be accomplished by mapping current audit exposure by payer, audit type, and service line, and prioritizing the highest dollar-at-risk claims for review and remediation. Additionally, providers should build robust workflows to manage audit requests, capture documentation, and respond within deadlines to retain revenues.
3. Outpatient Coding Worsens
Outpatient coding-related denials increased in 2025, rising 26% after a 126% spike in 2024, signaling their critical vulnerability. To slow this escalation, providers must begin treating coding integrity as a foundational risk area rather than an afterthought. This includes conducting targeted risk-based coding audits in outpatient service lines, focusing on training, review, and oversight of outpatient coding workflows, and ensuring that coding tools, documentation support, and coder oversight align with the heightened scrutiny, governance, and human oversight requirements.
4. Technology Unlocks Outcomes
There was a silver lining in the 2025 Benchmark Report: technology- and data-driven approaches are gaining traction and delivering measurable improvements, and revenue integrity teams are increasingly adopting data- and AI-driven approaches to unlock revenue opportunities and mitigate risk. Risk-based audits within the MDaudit platform increased by 25%, and pre-bill audits increased by 30%.
"Provider organizations that leverage data-driven platforms and deploy real-time, continuous risk monitoring can stay ahead of payers by better understanding real-time billing, coding, and payment trends," said Ramesh. "This allows them to take proactive action to educate providers and coders while addressing other issues."
Looking Ahead
Technology-including the responsible integration of artificial intelligence (AI) and real-time performance data shared across multiple functions-will continue to play an outsized role in driving competitive advantage and assuring financial resiliency in the year ahead. Integration of autonomous coding, predictive audit sampling, and workflow automation is expected to expand across the industry. Meanwhile:
Continuous risk monitoring tools will reduce payer audit response times by half and maintain tighter oversight of at-risk revenue through automation and centralized audit tracking.
Pairing automation with intelligent human oversight will drive measurable gains in accuracy, compliance, and speed.
AI-powered revenue integrity platforms will result in exponential lifts in operational efficiency and denial overturn success rates.
"The 2025 benchmark data makes clear that the margin for error in billing, coding, and audits has shrunk, and technology is becoming a differentiator," said Ramesh. "Organizations that adopt analytics, proactive audit/pre-bill workflows, and coding integrity will have a distinct advantage."
About the Report
The MDaudit 2025 Annual Benchmark Report is a comprehensive examination of real-world data representing the first three quarters of 2025, from a network of more than 1.2 million providers and over 4,500 facilities across 40+ states.
Download the MDaudit 2025Annual Benchmark Report.
About MDaudit
MDaudit is an award-winning AI-enhanced continuous risk monitoring platform and trusted revenue integrity partner to healthcare organizations nationwide. Working in the background, we deliver the insights you need to face the future with confidence. Our sustainable solution enables teams to achieve more with less, driving an efficient and compliant revenue cycle in a rapidly evolving environment. Learn more at www.mdaudit.com
###
Media Contact:
Rachel Driskell | [email protected]
SOURCE: MDaudit
View the original press release on ACCESS Newswire
A.Mahlangu--AMWN


